This is featured post 1 title
Replace these every slider sentences with your featured post descriptions.Go to Blogger edit html and find these sentences.Now replace these with your own descriptions.This theme is Bloggerized by Lasantha - Premiumbloggertemplates.com.

This is featured post 2 title
Replace these every slider sentences with your featured post descriptions.Go to Blogger edit html and find these sentences.Now replace these with your own descriptions.This theme is Bloggerized by Lasantha - Premiumbloggertemplates.com.

This is featured post 3 title
Replace these every slider sentences with your featured post descriptions.Go to Blogger edit html and find these sentences.Now replace these with your own descriptions.This theme is Bloggerized by Lasantha - Premiumbloggertemplates.com.

Kamis, 25 November 2010
Disorders
Posted by dvntr on 00.58
Anxiety or fear that interferes with normal functioning may be classified as an anxiety disorder.[7] Commonly recognized categories include specific phobias, generalized anxiety disorder, social anxiety disorder, panic disorder, agoraphobia, obsessive-compulsive disorder and post-traumatic stress disorder.
Other affective (emotion/mood) processes can also become disordered. Mood disorder involving unusually intense and sustained sadness, melancholia or despair is known as Major depression or Clinical depression (milder but still prolonged depression can be diagnosed as dysthymia). Bipolar disorder (also known as manic depression) involves abnormally "high" or pressured mood states, known as mania or hypomania, alternating with normal or depressed mood. Whether unipolar and bipolar mood phenomena represent distinct categories of disorder, or whether they usually mix and merge together along a dimension or spectrum of mood, is under debate in the scientific literature.[8]
Patterns of belief, language use and perception can become disordered (e.g. delusions, thought disorder, hallucinations). Psychotic disorders in this domain include schizophrenia, and delusional disorder. Schizoaffective disorder is a category used for individuals showing aspects of both schizophrenia and affective disorders. Schizotypy is a category used for individuals showing some of the characteristics associated with schizophrenia but without meeting cut-off criteria.
Personality—the fundamental characteristics of a person that influence his or her thoughts and behaviors across situations and time—may be considered disordered if judged to be abnormally rigid and maladaptive. Categorical schemes list a number of different such personality disorders, including those sometimes classed as eccentric (e.g. paranoid, schizoid and schizotypal personality disorders), to those sometimes classed as dramatic or emotional (antisocial, borderline, histrionic or narcissistic personality disorders) or those seen as fear-related (avoidant, dependent, or obsessive-compulsive personality disorders). If an inability to sufficiently adjust to life circumstances begins within three months of a particular event or situation, and ends within six months after the stressor stops or is eliminated, it may instead be classed as an adjustment disorder. There is an emerging consensus that so-called "personality disorders", like personality traits in general, actually incorporate a mixture of acute dysfunctional behaviors that resolve in short periods, and maladaptive temperamental traits that are more stable.[9] Furthermore, there are also non-categorical schemes that rate all individuals via a profile of different dimensions of personality rather than using a cut-off from normal personality variation, for example through schemes based on the Big Five personality traits.[10]
Eating disorders involve disproportionate concern in matters of food and weight.[7] Categories of disorder in this area include anorexia nervosa, bulimia nervosa, exercise bulimia or binge eating disorder.
Sleep disorders such as insomnia involve disruption to normal sleep patterns, or a feeling of tiredness despite sleep appearing normal.
Sexual and gender identity disorders may be diagnosed, including dyspareunia, gender identity disorder and ego-dystonic homosexuality. Various kinds of paraphilia are considered mental disorders (sexual arousal to objects, situations, or individuals that are considered abnormal or harmful to the person or others).
People who are abnormally unable to resist certain urges or impulses that could be harmful to themselves or others, may be classed as having an impulse control disorder, including various kinds of tic disorders such as Tourette's syndrome, and disorders such as kleptomania (stealing) or pyromania (fire-setting). Various behavioral addictions, such as gambling addiction, may be classed as a disorder. Obsessive-compulsive disorder can sometimes involve an inability to resist certain acts but is classed separately as being primarily an anxiety disorder.
The use of drugs (legal or illegal), when it persists despite significant problems related to the use, may be defined as a mental disorder termed substance dependence or substance abuse (a broader category than drug abuse). The DSM does not currently use the common term drug addiction and the ICD simply talks about "harmful use". Disordered substance use may be due to a pattern of compulsive and repetitive use of the drug that results in tolerance to its effects and withdrawal symptoms when use is reduced or stopped.
People who suffer severe disturbances of their self-identity, memory and general awareness of themselves and their surroundings may be classed as having a dissociative identity disorder, such as depersonalization disorder or Dissociative Identity Disorder itself (which has also been called multiple personality disorder, or "split personality"). Other memory or cognitive disorders include amnesia or various kinds of old age dementia.
A range of developmental disorders that initially occur in childhood may be diagnosed, for example autism spectrum disorders, oppositional defiant disorder and conduct disorder, and attention deficit hyperactivity disorder (ADHD), which may continue into adulthood.
Conduct disorder, if continuing into adulthood, may be diagnosed as antisocial personality disorder (dissocial personality disorder in the ICD). Popularist labels such as psychopath (or sociopath) do not appear in the DSM or ICD but are linked by some to these diagnoses.
Disorders appearing to originate in the body, but thought to be mental, are known as somatoform disorders, including somatization disorder and conversion disorder. There are also disorders of the perception of the body, including body dysmorphic disorder. Neurasthenia is an old diagnosis involving somatic complaints as well as fatigue and low spirits/depression, which is officially recognized by the ICD-10 but no longer by the DSM-IV.[11]
Factitious disorders, such as Munchausen syndrome, are diagnosed where symptoms are thought to be experienced (deliberately produced) and/or reported (feigned) for personal gain.
There are attempts to introduce a category of relational disorder, where the diagnosis is of a relationship rather than on any one individual in that relationship. The relationship may be between children and their parents, between couples, or others. There already exists, under the category of psychosis, a diagnosis of shared psychotic disorder where two or more individuals share a particular delusion because of their close relationship with each other.
Various new types of mental disorder diagnosis are occasionally proposed. Among those controversially considered by the official committees of the diagnostic manuals include self-defeating personality disorder, sadistic personality disorder, passive-aggressive personality disorder and premenstrual dysphoric disorder.
Two recent unique isolated proposals are solastalgia by Glenn Albrecht and hubris syndrome by David Owen. The application of the concept of mental illness to the phenomena described by these authors has in turn been critiqued by Seamus Mac Suibhne.[12]
Mental disorder
Posted by dvntr on 00.42
From Wikipedia, the free encyclopedia
Jump to: navigation, search
| Mental disorder | |
|---|---|
| Classification and external resources | |
 Eight women representing prominent mental diagnoses in the 19th century. (Armand Gautier) | |
| ICD-10 | F. |
| MeSH | D001523 |
The causes are often explained in terms of a diathesis-stress model or biopsychosocial model. In biological psychiatry, mental disorders are conceptualized as disorders of brain circuits likely caused by developmental processes shaped by a complex interplay of genetics and experience.[1]
Services are based in psychiatric hospitals or in the community. Diagnoses are made by psychiatrists or clinical psychologists using various methods, often relying on observation and questioning in interviews. Treatments are provided by various mental health professionals. Psychotherapy and psychiatric medication are two major treatment options as are social interventions, peer support and self-help. In some cases there may be involuntary detention and involuntary treatment where legislation allows.
Stigma and discrimination add to the suffering associated with the disorders, and have led to various social movements campaign for change.[clarification needed]
Classifications
Posted by dvntr on 00.40
Main article: Classification of mental disorders
The definition and classification of mental disorders is a key issue for mental health and for users and providers of mental health services. Most international clinical documents use the term "mental disorder". There are currently two widely established systems that classify mental disorders—ICD-10 Chapter V: Mental and behavioural disorders, part of the International Classification of Diseases produced by the World Health Organization (WHO), and the Diagnostic and Statistical Manual of Mental Disorders (DSM-IV) produced by the American Psychiatric Association (APA). Both list categories of disorder and provide standardized criteria for diagnosis. They have deliberately converged their codes in recent revisions so that the manuals are often broadly comparable, although significant differences remain. Other classification schemes may be used in non-western cultures (see, for example, the Chinese Classification of Mental Disorders), and other manuals may be used by those of alternative theoretical persuasions, for example the Psychodynamic Diagnostic Manual. In general, mental disorders are classified separately to neurological disorders, learning disabilities or mental retardation.Unlike most of the above systems, some approaches to classification do not employ distinct categories of disorder or dichotomous cut-offs intended to separate the abnormal from the normal. There is significant scientific debate about the different kinds of categorization and the relative merits of categorical versus non-categorical (or hybrid) schemes, with the latter including spectrum, continuum or dimensional systems.
Disorders
Posted by dvntr on 00.38
Anxiety or fear that interferes with normal functioning may be classified as an anxiety disorder.[7] Commonly recognized categories include specific phobias, generalized anxiety disorder, social anxiety disorder, panic disorder, agoraphobia, obsessive-compulsive disorder and post-traumatic stress disorder.
Other affective (emotion/mood) processes can also become disordered. Mood disorder involving unusually intense and sustained sadness, melancholia or despair is known as Major depression or Clinical depression (milder but still prolonged depression can be diagnosed as dysthymia). Bipolar disorder (also known as manic depression) involves abnormally "high" or pressured mood states, known as mania or hypomania, alternating with normal or depressed mood. Whether unipolar and bipolar mood phenomena represent distinct categories of disorder, or whether they usually mix and merge together along a dimension or spectrum of mood, is under debate in the scientific literature.[8]
Patterns of belief, language use and perception can become disordered (e.g. delusions, thought disorder, hallucinations). Psychotic disorders in this domain include schizophrenia, and delusional disorder. Schizoaffective disorder is a category used for individuals showing aspects of both schizophrenia and affective disorders. Schizotypy is a category used for individuals showing some of the characteristics associated with schizophrenia but without meeting cut-off criteria.
Personality—the fundamental characteristics of a person that influence his or her thoughts and behaviors across situations and time—may be considered disordered if judged to be abnormally rigid and maladaptive. Categorical schemes list a number of different such personality disorders, including those sometimes classed as eccentric (e.g. paranoid, schizoid and schizotypal personality disorders), to those sometimes classed as dramatic or emotional (antisocial, borderline, histrionic or narcissistic personality disorders) or those seen as fear-related (avoidant, dependent, or obsessive-compulsive personality disorders). If an inability to sufficiently adjust to life circumstances begins within three months of a particular event or situation, and ends within six months after the stressor stops or is eliminated, it may instead be classed as an adjustment disorder. There is an emerging consensus that so-called "personality disorders", like personality traits in general, actually incorporate a mixture of acute dysfunctional behaviors that resolve in short periods, and maladaptive temperamental traits that are more stable.[9] Furthermore, there are also non-categorical schemes that rate all individuals via a profile of different dimensions of personality rather than using a cut-off from normal personality variation, for example through schemes based on the Big Five personality traits.[10]
Eating disorders involve disproportionate concern in matters of food and weight.[7] Categories of disorder in this area include anorexia nervosa, bulimia nervosa, exercise bulimia or binge eating disorder.
Sleep disorders such as insomnia involve disruption to normal sleep patterns, or a feeling of tiredness despite sleep appearing normal.
Sexual and gender identity disorders may be diagnosed, including dyspareunia, gender identity disorder and ego-dystonic homosexuality. Various kinds of paraphilia are considered mental disorders (sexual arousal to objects, situations, or individuals that are considered abnormal or harmful to the person or others).
People who are abnormally unable to resist certain urges or impulses that could be harmful to themselves or others, may be classed as having an impulse control disorder, including various kinds of tic disorders such as Tourette's syndrome, and disorders such as kleptomania (stealing) or pyromania (fire-setting). Various behavioral addictions, such as gambling addiction, may be classed as a disorder. Obsessive-compulsive disorder can sometimes involve an inability to resist certain acts but is classed separately as being primarily an anxiety disorder.
The use of drugs (legal or illegal), when it persists despite significant problems related to the use, may be defined as a mental disorder termed substance dependence or substance abuse (a broader category than drug abuse). The DSM does not currently use the common term drug addiction and the ICD simply talks about "harmful use". Disordered substance use may be due to a pattern of compulsive and repetitive use of the drug that results in tolerance to its effects and withdrawal symptoms when use is reduced or stopped.
People who suffer severe disturbances of their self-identity, memory and general awareness of themselves and their surroundings may be classed as having a dissociative identity disorder, such as depersonalization disorder or Dissociative Identity Disorder itself (which has also been called multiple personality disorder, or "split personality"). Other memory or cognitive disorders include amnesia or various kinds of old age dementia.
A range of developmental disorders that initially occur in childhood may be diagnosed, for example autism spectrum disorders, oppositional defiant disorder and conduct disorder, and attention deficit hyperactivity disorder (ADHD), which may continue into adulthood.
Conduct disorder, if continuing into adulthood, may be diagnosed as antisocial personality disorder (dissocial personality disorder in the ICD). Popularist labels such as psychopath (or sociopath) do not appear in the DSM or ICD but are linked by some to these diagnoses.
Disorders appearing to originate in the body, but thought to be mental, are known as somatoform disorders, including somatization disorder and conversion disorder. There are also disorders of the perception of the body, including body dysmorphic disorder. Neurasthenia is an old diagnosis involving somatic complaints as well as fatigue and low spirits/depression, which is officially recognized by the ICD-10 but no longer by the DSM-IV.[11]
Factitious disorders, such as Munchausen syndrome, are diagnosed where symptoms are thought to be experienced (deliberately produced) and/or reported (feigned) for personal gain.
There are attempts to introduce a category of relational disorder, where the diagnosis is of a relationship rather than on any one individual in that relationship. The relationship may be between children and their parents, between couples, or others. There already exists, under the category of psychosis, a diagnosis of shared psychotic disorder where two or more individuals share a particular delusion because of their close relationship with each other.
Various new types of mental disorder diagnosis are occasionally proposed. Among those controversially considered by the official committees of the diagnostic manuals include self-defeating personality disorder, sadistic personality disorder, passive-aggressive personality disorder and premenstrual dysphoric disorder.
Two recent unique isolated proposals are solastalgia by Glenn Albrecht and hubris syndrome by David Owen. The application of the concept of mental illness to the phenomena described by these authors has in turn been critiqued by Seamus Mac Suibhne.[12]
Causes
Posted by dvntr on 00.30
Main article: Causes of mental disorders
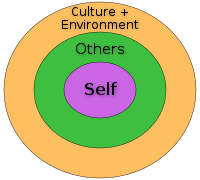
Mental disorders can arise from a combination of sources. In many cases there is no single accepted or consistent cause currently established. A common belief even to this day is that disorders result from genetic vulnerabilities exposed by environmental stressors. (see Diathesis-stress model). However, it is clear enough from a simple statistical analysis across the whole spectrum of mental health disorders at least in western cultures that there is a strong relationship between the various forms of severe and complex mental disorder in adulthood and the abuse (physical, sexual or emotional) or neglect of children during the developmental years. Child sexual abuse alone plays a significant role in the causation of a significant percentage of all mental disorders in adult females, most notable examples being eating disorders and borderline personality disorder.An eclectic or pluralistic mix of models may be used to explain particular disorders, and the primary paradigm of contemporary mainstream Western psychiatry is said to be the biopsychosocial (BPS) model, incorporating biological, psychological and social factors, although this may not always be applied in practice. Biopsychiatry has tended to follow a biomedical model, focusing on "organic" or "hardware" pathology of the brain. Psychoanalytic theories have continued to evolve alongside congitive-behavioural and systemic-family approaches been popular but are now less so. Evolutionary psychology may be used as an overall explanatory theory, and attachment theory is another kind of evolutionary-psychological approach sometimes applied in the context of mental disorders. A distinction is sometimes made between a "medical model" or a "social model" of disorder and disability.
Studies have indicated that genes often play an important role in the development of mental disorders, although the reliable identification of connections between specific genes and specific categories of disorder has proven more difficult. Environmental events surrounding pregnancy and birth have also been implicated. Traumatic brain injury may increase the risk of developing certain mental disorders. There have been some tentative inconsistent links found to certain viral infections,[13] to substance misuse, and to general physical health.
Abnormal functioning of neurotransmitter systems has been implicated, including serotonin, norepinephrine, dopamine and glutamate systems. Differences have also been found in the size or activity of certain brain regions in some cases. Psychological mechanisms have also been implicated, such as cognitive (e.g. reason), emotional processes, personality, temperament and coping style.
Social influences have been found to be important, including abuse, bullying and other negative or stressful life experiences. The specific risks and pathways to particular disorders are less clear, however. Aspects of the wider community have also been implicated, including employment problems, socioeconomic inequality, lack of social cohesion, problems linked to migration, and features of particular societies and cultures.
Gender-specific influences
Posted by dvntr on 00.29
Female-specific indicators of mental illness incorporate physical or sexual abuse, stress, loss of social network, rape and domestic violence, high progesterone oral contraceptives, and mood disorders during early reproductive years.[14] It is important to note that the intersection of biological, social, and behavioral health problems may result in exacerbated mental health issues. An investigation carried out by the US National Camorbidity Survey (NCS) showed that 5% of woman that had been exposed to a traumatic event went onto develop post-tramautic stress disorder (PTSD). It is also reported that women are the most vulnerable during the aftermath of a disaster. These circumstances increase the risk of poor physical health, anxiety, and depression which are all factors of mental health disorders. (Chandra P.S., et al. 2009). [15
Diagnosis
Posted by dvntr on 00.28
Many mental health professionals, particularly psychiatrists, seek to diagnose individuals by ascertaining their particular mental disorder. Some professionals, for example some clinical psychologists, may avoid diagnosis in favor of other assessment methods such as formulation of a client's difficulties and circumstances.[16] The majority of mental health problems are actually assessed and treated by family physicians during consultations, who may refer on for more specialist diagnosis in acute or chronic cases. Routine diagnostic practice in mental health services typically involves an interview (which may be referred to as a mental status examination), where judgments are made of the interviewee's appearance and behavior, self-reported symptoms, mental health history, and current life circumstances. The views of relatives or other third parties may be taken into account. A physical examination to check for ill health or the effects of medications or other drugs may be conducted. Psychological testing is sometimes used via paper-and-pen or computerized questionnaires, which may include algorithms based on ticking off standardized diagnostic criteria, and in rare specialist cases neuroimaging tests may be requested, but these methods are more commonly found in research studies than routine clinical practice.[17][18] Time and budgetary constraints often limit practicing psychiatrists from conducting more thorough diagnostic evaluations.[19] It has been found that most clinicians evaluate patients using an unstructured, open-ended approach, with limited training in evidence-based assessment methods, and that inaccurate diagnosis may be common in routine practice.[20] Mental illness involving hallucinations or delusions (especially schizophrenia) are prone to misdiagnosis in developing countries due to the presence of psychotic symptoms instigated by nutritional deficiencies. Comorbidity is very common in psychiatric diagnoses, i.e. the same person given a diagnosis in more than one category of disorder.
Management
Posted by dvntr on 00.26
Management
Main articles: Treatment of mental disorders and Services for mental disorders
Treatment and support for mental disorders is provided in psychiatric hospitals, clinics or any of a diverse range of community mental health services. In many countries services are increasingly based on a recovery model that is meant to support each individual's independence, choice and personal journey to regain a meaningful life, although individuals may be treated against their will in a minority of cases. There are a range of different types of treatment and what is most suitable depends on the disorder and on the individual. Many things have been found to help at least some people, and a placebo effect may play a role in any intervention or medication.[edit] Psychotherapy
A major option for many mental disorders is psychotherapy. There are several main types. Cognitive behavioral therapy (CBT) is widely used and is based on modifying the patterns of thought and behavior associated with a particular disorder. Psychoanalysis, addressing underlying psychic conflicts and defenses, has been a dominant school of psychotherapy and is still in use. Systemic therapy or family therapy is sometimes used, addressing a network of significant others as well as an individual. Some psychotherapies are based on a humanistic approach. There are a number of specific therapies used for particular disorders, which may be offshoots or hybrids of the above types. Mental health professionals often employ an eclectic or integrative approach. Much may depend on the therapeutic relationship, and there may be problems with trust, confidentiality and engagement.[edit] Medication
A major option for many mental disorders is psychiatric medication and there are several main groups. Antidepressants are used for the treatment of clinical depression as well as often for anxiety and other disorders. Anxiolytics are used for anxiety disorders and related problems such as insomnia. Mood stabilizers are used primarily in bipolar disorder. Antipsychotics are mainly used for psychotic disorders, notably for positive symptoms in schizophrenia. Stimulants are commonly used, notably for ADHD.Despite the different conventional names of the drug groups, there may be considerable overlap in the disorders for which they are actually indicated, and there may also be off-label use of medications. There can be problems with adverse effects of medication and adherence to them, and there is also criticism of pharmaceutical marketing and professional conflicts of interest.
[edit] Other
Electroconvulsive therapy (ECT) is sometimes used in severe cases when other interventions for severe intractable depression have failed. Psychosurgery is considered experimental but is advocated by certain neurologists in certain rare cases.[21][22]Counseling (professional) and co-counseling (between peers) may be used. Psychoeducation programs may provide people with the information to understand and manage their problems. Creative therapies are sometimes used, including music therapy, art therapy or drama therapy. Lifestyle adjustments and supportive measures are often used, including peer support, self-help groups for mental health and supported housing or supported employment (including social firms). Some advocate dietary supplements.[23]
[edit] Prognosis
Prognosis depends on the disorder, the individual and numerous related factors. Some disorders are transient, while others may last a lifetime. Some disorders may be very limited in their functional effects, while others may involve substantial disability and support needs. The degree of ability or disability may vary across different life domains. Continued disability has been linked to institutionalization, discrimination and social exclusion as well as to the inherent properties of disorders.Even those disorders often considered the most serious and intractable have varied courses. Long-term international studies of schizophrenia have found that over a half of individuals recover in terms of symptoms, and around a fifth to a third in terms of symptoms and functioning, with some requiring no medication. At the same time, many have serious difficulties and support needs for many years, although "late" recovery is still possible. The World Health Organization concluded that the long-term studies' findings converged with others in "relieving patients, carers and clinicians of the chronicity paradigm which dominated thinking throughout much of the 20th century."[24][25] Around half of people initially diagnosed with bipolar disorder achieve syndromal recovery (no longer meeting criteria for the diagnosis) within six weeks, and nearly all achieve it within two years, with nearly half regaining their prior occupational and residential status in that period. However, nearly half go on to experience a new episode of mania or major depression within the next two years.[26] Functioning has been found to vary, being poor during periods of major depression or mania but otherwise fair to good, and possibly superior during periods of hypomania in Bipolar II.[27]
Some mental disorders are linked, on average, to increased rates of attempted and/or completed suicide or self-harm.
Despite often being characterized in purely negative terms, some mental states labeled as disorders can also involve above-average creativity, non-conformity, goal-striving, meticulousness, or empathy.[28] In addition, the public perception of the level of disability associated with mental disorders can change.[29]
[edit] Epidemiology
Main article: Prevalence of mental disorders
Mental disorders are common. World wide more than one in three people in most countries report sufficient criteria for at least one at some point in their life.[30] In the United States 46% qualifies for a mental illness at some point.[31] An ongoing survey indicates that anxiety disorders are the most common in all but one country, followed by mood disorders in all but two countries, while substance disorders and impulse-control disorders were consistently less prevalent.[32] Rates varied by region.[33] Such statistics are widely believed to be underestimates, due to poor diagnosis (especially in countries without affordable access to mental health services) and low reporting rates, in part because of the predominant use of self-report data rather than semi-structured instruments.[citation needed] Actual lifetime prevalence rates for mental disorders are estimated to be between 65% and 85%.[citation needed]A review of anxiety disorder surveys in different countries found average lifetime prevalence estimates of 16.6%, with women having higher rates on average.[34] A review of mood disorder surveys in different countries found lifetime rates of 6.7% for major depressive disorder (higher in some studies, and in women) and 0.8% for Bipolar I disorder.[35]
In the United States the frequency of disorder is: anxiety disorder (28.8%), mood disorder (20.8%), impulse-control disorder (24.8%) or substance use disorder (14.6%).[36][37][38]
A 2004 cross-Europe study found that approximately one in four people reported meeting criteria at some point in their life for at least one of the DSM-IV disorders assessed, which included mood disorders (13.9%), anxiety disorders (13.6%) or alcohol disorder (5.2%). Approximately one in ten met criteria within a 12-month period. Women and younger people of either gender showed more cases of disorder.[39] A 2005 review of surveys in 16 European countries found that 27% of adult Europeans are affected by at least one mental disorder in a 12 month period.[40]
An international review of studies on the prevalence of schizophrenia found an average (median) figure of 0.4% for lifetime prevalence; it was consistently lower in poorer countries.[41]
Studies of the prevalence of personality disorders (PDs) have been fewer and smaller-scale, but one broad Norwegian survey found a five-year prevalence of almost 1 in 7 (13.4%). Rates for specific disorders ranged from 0.8% to 2.8%, differing across countries, and by gender, educational level and other factors.[42] A US survey that incidentally screened for personality disorder found a rate of 14.79%.[43]
Approximately 7% of a preschool pediatric sample were given a psychiatric diagnosis in one clinical study, and approximately 10% of 1- and 2-year-olds receiving developmental screening have been assessed as having significant emotional/behavioral problems based on parent and pediatrician reports.[44]
While rates of psychological disorders are the same for men and women, women have twice the rate of depression than men.[45] Each year 73 million women are afflicted with major depression, and suicide is ranked 7th as the cause of death for women between the ages of 20-59. Depressive disorders account for close to 41.9% of the disability from neuropsychiatric disorders among women compared to 29.3% among men.[46]
[edit] History
History
Posted by dvntr on 00.23
Main article: History of mental disorders
[edit] Ancient civilizations
Ancient civilizations described and treated a number of mental disorders. The Greeks coined terms for melancholy, hysteria and phobia and developed the humorism theory. Psychiatric theories and treatments developed in Persia, Arabia and the Muslim Empire, particularly in the medieval Islamic world from the 8th century, where the first psychiatric hospitals were built.[edit] Europe
[edit] Middle Ages
Conceptions of madness in the Middle Ages in Christian Europe were a mixture of the divine, diabolical, magical and humoral, as well as more down to earth considerations. In the early modern period, some people with mental disorders may have been victims of the witch-hunts but were increasingly admitted to local workhouses and jails or sometimes to private madhouses. Many terms for mental disorder that found their way into everyday use first became popular in the 16th and 17th centuries.[edit] Eighteenth century
By the end of the 17th century and into the Enlightenment, madness was increasingly seen as an organic physical phenomenon with no connection to the soul or moral responsibility. Asylum care was often harsh and treated people like wild animals, but towards the end of the 18th century a moral treatment movement gradually developed. Clear descriptions of some syndromes may be rare prior to the 19th century.[edit] Nineteenth century
Industrialization and population growth led to a massive expansion of the number and size of insane asylums in every Western country in the 19th century. Numerous different classification schemes and diagnostic terms were developed by different authorities, and the term psychiatry was coined, though medical superintendents were still known as alienists.[edit] Twentieth century
The turn of the 20th century saw the development of psychoanalysis, which would later come to the fore, along with Kraepelin's classification scheme. Asylum "inmates" were increasingly referred to as "patients", and asylums renamed as hospitals.[edit] Europe and the U.S.
In the 20th century in the United States, a mental hygiene movement developed, aiming to prevent mental disorders. Clinical psychology and social work developed as professions. World War I saw a massive increase of conditions that came to be termed "shell shock".World War II saw the development in the U.S. of a new psychiatric manual for categorizing mental disorders, which along with existing systems for collecting census and hospital statistics led to the first Diagnostic and Statistical Manual of Mental Disorders (DSM). The International Classification of Diseases (ICD) followed suit with a section on mental disorders. The term stress, having emerged out of endocrinology work in the 1930s, was increasingly applied to mental disorders.
Electroconvulsive therapy, insulin shock therapy, lobotomies and the "neuroleptic" chlorpromazine came to be used by mid-century. An antipsychiatry movement came to the fore in the 1960s. Deinstitutionalization gradually occurred in the West, with isolated psychiatric hospitals being closed down in favor of community mental health services. A consumer/survivor movement gained momentum. Other kinds of psychiatric medication gradually came into use, such as "psychic energizers" and lithium. Benzodiazepines gained widespread use in the 1970s for anxiety and depression, until dependency problems curtailed their popularity.
Advances in neuroscience and genetics led to new research agendas. Cognitive behavioral therapy was developed. The DSM and then ICD adopted new criteria-based classifications, and the number of "official" diagnoses saw a large expansion. Through the 1990s, new SSRI antidepressants became some of the most widely prescribed drugs in the world. Also during the 1990s, a recovery model developed.
Society and culture
Posted by dvntr on 00.22
Different societies or cultures and even different individuals in a culture can disagree as to what constitutes optimal versus pathological biological and psychological functioning. Research has demonstrated that cultures vary in the relative importance placed on, for example, happiness, autonomy, or social relationships for pleasure. Likewise, the fact that a behavior pattern is valued, accepted, encouraged, or even statistically normative in a culture does not necessarily mean that it is conducive to optimal psychological functioning.
People in all cultures find some behaviors bizarre or even incomprehensible. But just what they feel is bizarre or incomprehensible is ambiguous and subjective.[47] These differences in determination can become highly contentious.
The process by which conditions and difficulties come to be defined and treated as medical conditions and problems, and thus come under the authority of doctors and other health professionals, is known as medicalization or pathologization.
In the scientific and academic literature on the definition or classification of mental disorder, one extreme argues that it is entirely a matter of value judgements (including of what is normal) while another proposes that it is or could be entirely objective and scientific (including by reference to statistical norms).[48] Common hybrid views argue that the concept of mental disorder is objective but a "fuzzy prototype" that can never be precisely defined, or alternatively that it inevitably involves a mix of scientific facts and subjective value judgments.[49
Professions and fields
Posted by dvntr on 00.21
Main article: Mental health professional
A number of professions have developed that specialize in the treatment of mental disorders, including the medical speciality of psychiatry (including psychiatric nursing),[50][51][52] a subset of psychology known as clinical psychology,[53] social work,[54] as well as mental health counselors, marriage and family therapists, psychotherapists, counselors and public health professionals. Those with personal experience of using mental health services are also increasingly involved in researching and delivering mental health services and working as mental health professionals.[55][56][57][58] The different clinical and scientific perspectives draw on diverse fields of research and theory, and different disciplines may favor differing models, explanations and goals.Movements
Posted by dvntr on 00.18
The consumer/survivor movement (also known as user/survivor movement) is made up of individuals (and organizations representing them) who are clients of mental health services or who consider themselves "survivors" of mental health services. The movement campaigns for improved mental health services and for more involvement and empowerment within mental health services, policies and wider society.[59][60][61] Patient advocacy organizations have expanded with increasing deinstitutionalization in developed countries, working to challenge the stereotypes, stigma and exclusion associated with psychiatric conditions. An antipsychiatry movement fundamentally challenges mainstream psychiatric theory and practice, including asserting that psychiatric diagnoses of mental illnesses are neither real nor useful.[
Intangible experiences
Posted by dvntr on 00.17
Religious, spiritual, or transpersonal experiences and beliefs are typically not defined as disordered, especially if widely shared, despite meeting many criteria of delusional or psychotic disorders.[65][66] Even when a belief or experience can be shown to produce distress or disability—the ordinary standard for judging mental disorders—the presence of a strong cultural basis for that belief, experience, or interpretation of experience, generally disqualifies it from counting as evidence of mental disorder.